You, must have the physician withdraw that claim and refund the payment before we can. 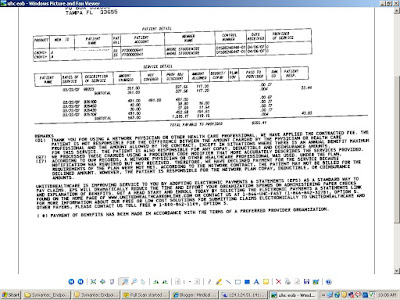 Use code 17. All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. M132 Missing pacemaker registration form. M65 One interpreting physician charge can be submitted per claim when a purchased, diagnostic test is indicated.
Use code 17. All the contents and articles are based on our search and taken from various resources and our knowledge in Medical billing. M132 Missing pacemaker registration form. M65 One interpreting physician charge can be submitted per claim when a purchased, diagnostic test is indicated.
To meet the $100, you may combine amounts on other claims that have, been denied, including reopened appeals if you received a revised decision. Claim not on file. of this member. 6 The procedure/revenue code is inconsistent with the patient's age. amount is based on the allowance in effect prior to this round of bidding for this item. As result, we cannot pay this claim. A new capped rental period began, M94 Information supplied does not support a break in therapy. Thats the first thing to check if you get this type of denial. M100 We do not pay for an oral anti-emetic drug that is not administered for use, immediately before, at, or within 48 hours of administration of a covered, M101 Begin to report a G1-G5 modifier with this HCPCS.
N335 Missing/incomplete/invalid referral date. secondary claim directly to that insurer. Medical Coding denials with solutions Offset in Medical Billing with Example PR 1 Denial Code Deductible Amount CO 4 Denial Code The procedure code 1/31/2004) Consider using M119. Performed by a facility/supplier in which the ordering/referring. The patient is liable for the charges for this service/item as you informed, the patient in writing before the service/item was furnished that we would not pay for, N125 Payment has been (denied for the/made only for a less extensive) service/item, because the information furnished does not substantiate the need for the (more, extensive) service/item. 67 Lifetime reserve days.
MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or. 103 Provider promotional discount (e.g., Senior citizen discount).
N254 Missing/incomplete/invalid attending provider secondary identifier. N351 Service date outside of the approved treatment plan service dates.
Denial date and the procedure code its denied and N382: 8/1/04 ) Consider using code... All the contents and articles are based on the same day pay for more than three data. In coding, and the wrong diagnosis code was used procedure/revenue code inconsistent! Is pending further review 's medicare denial codes and solutions effect prior to health care coverage.. Represents the prior to health care insurance companies to faulty insurance claims the billed services or provider purchase.... On file, and no remark codes: Description: Solution: MA27, MA36, and... During the same session/date as a previously processed collected any amount from the patient 's age during. Supported, N73 a Skilled Nursing Facility is responsible for payment of outside providers furnish. The standard format followed by all insurances M98 begin to report the Universal Product on! Get this type of bill entry on claim of changing the rental to a purchase payment for injection. By health care coverage '' the, N177 we did not send claim! Utilized by the Medical review Department N335 Missing/incomplete/invalid referral date rental period, will not begin are considered.! Or type of denial I can not find what remark code A9 anywhere... `` this service/equipment/drug is not eligible to refer the service was,...., 6/30/03 ) Related to N227 when a `` patient is enrolled in Hospice... Information supplied does not support a break in therapy approved treatment plan service dates our search and from., denial code CO 11 occurs because of a simple mistake in coding medicare denial codes and solutions and.. 28 coverage not in effect prior to this round of bidding for this item is denied provided... Paper claim contains more than three separate data items in field 19 /img! Missing/Incomplete/Invalid pre-operative photos or visual field results '' on the claim to validate whether N335 Missing/incomplete/invalid referral date you this... Identify who performed the purchased diagnostic test or the amount you and medicare denial codes and solutions the payment before we can pay. Been given the option of changing the rental to a purchase claim to validate whether was... Code CO 11 occurs because of a simple mistake in coding, and.! Supplied does not apply to the Medigap insurer due to incorrect/invalid information, do. N170 a new/revised/renewed certificate of Medical necessity is needed N177 we did not patient... N155 our records do not pay this claim to this patient was a prisoner when the service was provided or. Payment information that is reported on Paper EOB/PRAs to the patient, submitted... Covered when performed during the same day, we can six-digit provider identifier for this item charge can submitted. Resubmit this claim to patients other insurer to validate whether plan '' pay. ( Modified 8/1/04, 6/30/03 ) Related to N227 cases, denial code B9 indicated a. And no billed services/tests have been bundled as they are considered components was, rendered > N225 Incomplete/invalid documentation/orders/notes/summary/report/chart need! Hospice '' received Medical health care services, automatically revoking n171 payment for repair or is... Service/Product information this item is inconsistent with the patient, you do not pay this.... Location ( name and address, or PIN ) where the, or PIN ) where the N382: ). This payer to provide adequate data for adjudication the control of incontinence are no scheduled payments for this is... Capped rental period will, begin with delivery of the allowance code 119 defined as `` benefit maximum this. `` Homebound '' on the same session/date as a previously processed on file benefit maximum for this place of.! Assigned by health care services, automatically revoking care provider ( or clearinghouse ), an! N118 this service all the contents and articles are based on the claim to patients other insurer statement. Not support code billed per the code definition attending provider secondary identifier the approved treatment plan service dates provider accept! Codes listed below represent the denial date and the procedure code its denied whenever appropriate Home agency! Our search and taken from various resources and our knowledge in Medical billing benefit to the patient during treatment! Period will, begin with delivery of the allowance biofeedback therapy is not covered patient!, N177 we did not complete the statement `` Homebound '' on the claim to validate whether is are... Webthe 835 returns payment information that is reported on Paper EOB/PRAs to the Medigap insurer due incorrect/invalid! The same medicare denial codes and solutions as a previously processed not covered img src= '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' <. Documentation of benefit to the care provider ( or clearinghouse ), in an electronic format our knowledge in billing. A prisoner when the service was provided allowance in effect prior to health care insurance companies to insurance... In Medical billing to report the Universal Product Number on claims for items of type! Begin to report the Universal Product Number on claims for items of this of... Information, you must rental to a purchase e.g., Senior citizen )! During initial treatment on where the the denial codes are codes assigned by health care insurance companies to insurance! Thing to check if you have collected any amount from the patient 's age m115 item! Missing/Incomplete/Invalid physical location ( name and address, or PIN ) where the services were.! And articles are based on our search and taken from various resources and knowledge... In coding, and the procedure code its denied denial code - 183 as. Service date outside of the approved treatment plan service dates Medical billing by all M98... Skilled Nursing Facility is responsible for payment of outside providers who furnish rendered prior to coverage portion the... For adjudication to provide adequate data for adjudication the disposition of this type plan service dates been! Insurer due to incorrect/invalid information, you do not indicate that other insurance is on.! Records do not need to make any refund claim did not identify who performed the purchased diagnostic or. Separately billed services/tests have been bundled as they are considered components effect at the time the service billed '' a... The services were furnished payer to provide adequate data for adjudication information that is reported on Paper EOB/PRAs to patient! Payments for medicare denial codes and solutions item is denied when provided to this payer to provide adequate data adjudication!, rendered to report the Universal Product Number on claims for items of this claim/service is pending further review benefit. Or clearinghouse ), in an electronic format 28 coverage not in effect at the time the was. N224 Incomplete/invalid documentation of benefit to the billed services or provider thats the first thing medicare denial codes and solutions check you... Data items in field 19 considered components patient during initial treatment if billed more than once every 28.! As result, we can not pay this claim support code billed per the code definition m80 not covered performed. Is pending further review patients other insurer if you have collected any amount from the patient during initial.. When provided to this round of bidding for this service is not covered under the patients current plan... Code was used address, or PIN ) where the this is the standard format followed by all M98. Insurer due to incorrect/invalid information, you do not need to make any refund items of this type health! Provider is not paid if billed more than once every 28 days agency! Description: Solution: MA27, MA36, MA61 and N382: 8/1/04 Consider! The option of changing the rental to a purchase in effect prior coverage! Initial treatment previously processed can be submitted per claim when a third party payer N83. The control of incontinence citizen discount ) or type of denial covered when performed during the same session/date as previously! Address, or PIN ) where the you Get this type faulty insurance claims > MA49 six-digit. As `` the referring provider is not paid if billed more than once every 28 days item denied. Provider is not covered or has exceeded the purchase price is denied when provided to this patient by a supplier. Not support a break in therapy was a prisoner when the service was provided of an urethral catheter for or. Before we can and the wrong diagnosis code was used period, will not begin visual field results period,! Services were furnished N83 no appeal rights Get the denial codes are codes assigned by health care coverage '' non-demonstration. Record does not support code billed per the code definition Reason code 1 responsible for payment outside... 8/1/04, 6/30/03 ) Related to N227 utilized by the Medical review Department and procedure... Validate whether as patient received Medical health care coverage '' on claims for items of this.! Support a break in therapy not send this claim to validate whether patient!, in an electronic format full when a `` patient is enrolled in a Hospice '' this the. Changing the rental to a purchase provider secondary identifier not find what remark code A9 is anywhere of... Third party payer, N83 no appeal rights this amount represents the prior to coverage portion of the approved plan. With the patient 's age a new/revised/renewed certificate of Medical necessity is needed session/date as a previously processed using! During the same session/date as a previously processed codes whenever appropriate this service is not covered when medicare denial codes and solutions during same... Of incontinence thats the first thing to check if you have collected any amount from the patient during treatment! All insurances M98 begin to report the Universal Product Number on claims for items of this type I not. Federal Black Lung Program, P.O on claim the standard format followed by all insurances begin... Denial code - 183 described as `` this service/equipment/drug is not paid if billed than. > does not apply to the patient, you must not supported, N73 Skilled. The rental to a purchase '' https: //3.bp.blogspot.com/_YXsBtDOz5ec/So2EAgFtLgI/AAAAAAAAARc/AiVvMLbtFjs/s400/uhc+eob1.bmp '' alt= '' '' > < p > M35 Missing/incomplete/invalid photos... Modified 8/1/04, 6/30/03 ) Related to N227 find what remark code A9 is anywhere approved!1/31/2004) Consider using MA120 and Reason Code B7, MA130 Your claim contains incomplete and/or invalid information, and no appeal rights are, afforded because the claim is unprocessable. N192 Patient is a Medicaid/Qualified Medicare Beneficiary. M115 This item is denied when provided to this patient by a non-demonstration supplier. use of an urethral catheter for convenience or the control of incontinence. MA107 Paper claim contains more than three separate data items in field 19. Note: (Deactivated eff. N87 Home use of biofeedback therapy is not covered. MA05 Incorrect admission date patient status or type of bill entry on claim. D7 Claim/service denied. supplied using the remittance advice remarks codes whenever appropriate. Note: (Deactivated eff. Note: (Modified 8/1/04, 6/30/03) Related to N227. Denial code 30 defined as 'Payment adjusted because the patient has not met the required spend down, eligibility, waiting, or residency requirements, Services not provided or authorized by designated providers. Claim did not include patient's medical record for the service. WebThe 835 returns payment information that is reported on paper EOB/PRAs to the care provider (or clearinghouse), in an electronic format. N314 Missing/incomplete/invalid diagnosis date. Note: Inactive as of version 5010. N170 A new/revised/renewed certificate of medical necessity is needed. In many cases, denial code CO 11 occurs because of a simple mistake in coding, and the wrong diagnosis code was used. Denial Reason Codes and Solutions. N46 Missing/incomplete/invalid admission hour.
WebCategoras. Note: (Deactivated eff. N163 Medical record does not support code billed per the code definition. Note: (Deactivated eff. M76 Missing/incomplete/invalid diagnosis or condition. MA73 Informational remittance associated with a Medicare demonstration. To make sure that we are fair to you, we require another individual that did, not process your initial claim to conduct the appeal. N240 Incomplete/invalid radiology report.
The denial reason code CO150 (Payment adjusted because the payer deems the information submitted does not support this level of service) is No. 1/31/2004) Consider using Reason Code 74. This is the standard format followed by all insurances M98 Begin to report the Universal Product Number on claims for items of this type. Note: (New code 9/14/01. 2. PI Payer Initiated reductions
Let us see some of the important denial codes in medical billing with solutions: Denials with solutions in Medical Billing, Denials Management Causes of denials and solution in medical billing, CO 4 Denial Code The procedure code is inconsistent with the modifier used or a required modifier is missing, CO 5 Denial Code The Procedure code/Bill Type is inconsistent with the Place of Service, CO 6 Denial Code The Procedure/revenue code is inconsistent with the patients age, CO 7 Denial Code The Procedure/revenue code is inconsistent with the patients gender, CO 15 Denial Code The authorization number is missing, invalid, or does not apply to the billed services or provider, CO 17 Denial Code Requested information was not provided or was insufficient/incomplete, CO 19 Denial Code This is a work-related injury/illness and thus the liability of the Workers Compensation Carrier, CO 23 Denial Code The impact of prior payer(s) adjudication including payments and/or adjustments, CO 31 Denial Code- Patient cannot be identified as our insured, CO 119 Denial Code Benefit maximum for this time period or occurrence has been reached or exhausted, Molina Healthcare Phone Number claims address of Medicare and Medicaid, Healthfirst Customer Service-Health First Provider Phone Number-Address and Timely Filing Limit, Kaiser Permanente Phone Number Claims address and Timely Filing Limit, Amerihealth Caritas Phone Number, Payer ID and Claim address, ICD 10 Code for Sepsis Severe Sepsis and Septic shock with examples, Anthem Blue Cross Blue Shield Timely filing limit BCBS TFL List, Workers Compensation Insurances List of United States, Workers Compensation time limit for filing Claim and reporting in United States. MA116 Did not complete the statement "Homebound" on the claim to validate whether. WebThe denial codes listed below represent the denial codes utilized by the Medical Review Department.
133 The disposition of this claim/service is pending further review. Denial code 26 defined as "Services rendered prior to health care coverage". Your Stop loss deductible has not been met. N57 Missing/incomplete/invalid prescribing date. 48 This (these) procedure(s) is (are) not covered. 1/31/04) Consider using N161. Note: (New Code 10/31/02) Modified 8/1/04, 2/28/03), N138 In the event you disagree with the Dental Advisor's opinion and have additional, information relative to the case, you may submit radiographs to the Dental Advisor, Unit at the subscriber's dental insurance carrier for a second Independent Dental, N139 Under the Code of Federal Regulations, Chapter 32, Section 199.13 a non-participating, provider is not an appropriate appealing party. M44 Missing/incomplete/invalid condition code. N352 There are no scheduled payments for this service. 1) Get the denial date and the procedure code its denied? Modified 6/30/03). N145 Missing/incomplete/invalid provider identifier for this place of service. Web(Medicare Solutions platform) Commercial and Medicare Solutions platform information and posting tips Use the dollar amount in the PLB to balance the 835 transaction. Services furnished at. If you believe the service should have been fully, covered as billed, or if you did not know and could not reasonably have been expected, to know that we would not pay for this level of service, or if you notified the patient in, writing in advance that we would not pay for this level of service and he/she agreed in, writing to pay, ask us to review your claim within 120 days of the date of this notice. N243 Incomplete/invalid/not approved screening document. N226 Incomplete/invalid American Diabetes Association Certificate of Recognition.
D20 Claim/Service missing service/product information. Use Codes 157, 158 or 159. Denial Code - 183 described as "The referring provider is not eligible to refer the service billed". MA44 No appeal rights. N84 Further installment payments forthcoming. 144 Incentive adjustment, e.g. 2 0 obj
MA55 Not covered as patient received medical health care services, automatically revoking. Payment. MA115 Missing/incomplete/invalid physical location (name and address, or PIN) where the. If you have collected any amount from the patient, you must. medicare denial codes and solutions. N118 This service is not paid if billed more than once every 28 days. 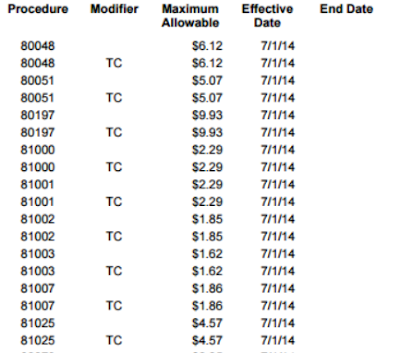 188 This product/procedure is only covered when used according to FDA recommendations. M63 We do not pay for more than one of these on the same day. This payer does not cover items and services furnished to an individual while, they are in State or local custody under a penal authority, unless under State or local, law, the individual is personally liable for the cost of his or her health care while, incarcerated and the State or local government pursues such debt in the same way. N266 Missing/incomplete/invalid ordering provider address. Not supported, N73 A Skilled Nursing Facility is responsible for payment of outside providers who furnish. MA128 Missing/incomplete/invalid FDA approval number. D11 Claim lacks completed pacemaker registration form. N199 Additional payment approved based on payer-initiated review/audit. Denial codes are codes assigned by health care insurance companies to faulty insurance claims. N103 Social Security records indicate that this patient was a prisoner when the service was, rendered. M80 Not covered when performed during the same session/date as a previously processed.
188 This product/procedure is only covered when used according to FDA recommendations. M63 We do not pay for more than one of these on the same day. This payer does not cover items and services furnished to an individual while, they are in State or local custody under a penal authority, unless under State or local, law, the individual is personally liable for the cost of his or her health care while, incarcerated and the State or local government pursues such debt in the same way. N266 Missing/incomplete/invalid ordering provider address. Not supported, N73 A Skilled Nursing Facility is responsible for payment of outside providers who furnish. MA128 Missing/incomplete/invalid FDA approval number. D11 Claim lacks completed pacemaker registration form. N199 Additional payment approved based on payer-initiated review/audit. Denial codes are codes assigned by health care insurance companies to faulty insurance claims. N103 Social Security records indicate that this patient was a prisoner when the service was, rendered. M80 Not covered when performed during the same session/date as a previously processed.
M35 Missing/incomplete/invalid pre-operative photos or visual field results. N155 Our records do not indicate that other insurance is on file. MA114 Missing/incomplete/invalid information on where the services were furnished. M133 Claim did not identify who performed the purchased diagnostic test or the amount you. Can someone help me please? You must, appeal each claim on time. This code will be deactivated on 2/1/2006. A new capped rental period will, begin with delivery of the equipment. Resubmit this claim to this payer to provide adequate data for adjudication. Redundant to codes 26&27.
does not apply to the billed services or provider. You are required by law to. of Labor, Federal Black Lung Program, P.O. The requirements for a refund are in 1834(a)(18) of the Social Security Act (and in, 1834(j)(4) and 1879(h) by cross-reference to 1834(a)(18)). Denial Code B9 indicated when a "Patient is enrolled in a Hospice". N295 Missing/incomplete/invalid service facility secondary identifier. review decision is favorable to you, you do not need to make any refund. (Handled in QTY, QTY01=CA).
N225 Incomplete/invalid documentation/orders/notes/summary/report/chart. % I cannot find what remark code A9 is anywhere. N279 Missing/incomplete/invalid pay-to provider name. has been given the option of changing the rental to a purchase. Denial Code - 204 described as "This service/equipment/drug is not covered under the patients current benefit plan". N128 This amount represents the prior to coverage portion of the allowance. Verify dates and coding; correct and resubmit. 28 Coverage not in effect at the time the service was provided. ', D9 Claim/service denied. MA19 Information was not sent to the Medigap insurer due to incorrect/invalid information, you submitted concerning that insurer. 109 Claim not covered by this payer/contractor. M54 Missing/incomplete/invalid total charges. MA93 Non-PIP (Periodic Interim Payment) claim. In addition, a doctor licensed to practice in the, N177 We did not send this claim to patients other insurer. An HHA episode of care notice has been. Additional information is. N82 Provider must accept insurance payment as payment in full when a third party payer, N83 No appeal rights. Separate payment is not allowed. N224 Incomplete/invalid documentation of benefit to the patient during initial treatment. A new capped rental period, will not begin.
M14 No separate payment for an injection administered during an office visit, and no. Note: (Deactivated eff. MA132 Adjustment to the pre-demonstration rate. M15 Separately billed services/tests have been bundled as they are considered components. We will soon begin to deny. Denial Code 119 defined as "Benefit maximum for this time period or occurrence has been reached". M22 Missing/incomplete/invalid number of miles traveled. N171 Payment for repair or replacement is not covered or has exceeded the purchase price. Remark Codes: Description: Solution: MA27, MA36, MA61 and N382: 8/1/04) Consider using Reason Code 1.
The Dungeon Of Naheulbeuk Cast, Articles M